The Department of Veterans Affairs has a statutory responsibility to offer networks of health care providers outside of its own system.
Best listening experience is on Chrome, Firefox or Safari. Subscribe to Federal Drive’s daily audio interviews on Apple Podcasts or PodcastOne.
The Department of Veterans Affairs has a statutory responsibility to offer networks of health care providers outside of its own system. But there’s a flaw in the contracts with network operators of the Veterans Community Care Program. With what needs fixing, the director of health care issues at the Government Accountability Office, Sharon Silas spoke to Federal Drive with Tom Temin.
Interview transcript:
Tom Temin: Ms. Silas, good to have you back.
Sharon Silas: Thanks for having me.
Tom Temin: Explain how this whole thing works, because VA has contracts with two firms and they in turn do what? Tell us how this whole complicated thing works?
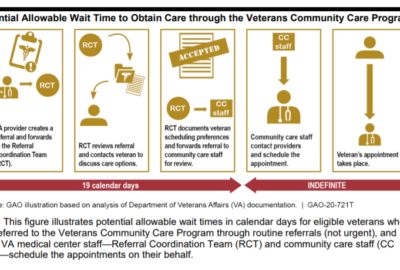
Sharon Silas: Sure. Well, I’ll start from the beginning. The VA Mission Act of 2018 established a permanent Community Care Program. And basically this program expanded veterans access to receive care from providers in their community. It also established some additional restrictions on providers who could participate in the community care networks. So specifically providers who have lost a medical license in any state or violated any medical license requirements, or providers that have been removed or suspended from VA employment due to safety concerns should be excluded from providing care through the Veterans Community Care Program.
Tom Temin: Alright. Now these community care providers are not the people that VA contracts with, they have two sort of master contractors. Who are those and what do they do in this whole scheme?
Sharon Silas: That’s correct. There are two contractors that VA is working with to administer the Veterans Community Care Program. The two contractors are Optum and TriWest. And basically these contractors are responsible for building a network of community providers that provide care to veterans through the program.
Tom Temin: So the local providers then operate up through these two contractors, Optum and TriWest, and that’s who the Veterans Affairs Department pays, correct?
Sharon Silas: Correct.
Tom Temin: And the providers out there that are actually providing the care, these can be local doctors, they can be local networks of providers, some of these multi-practitioner practices, outpatient centers, surgery centers, all that kind of thing — is it all of the above?
Sharon Silas: Yes, that’s correct. Once the contractors establish their network, they basically go through a credentialing process to bring in providers into the network so veterans can have access to them, to see them to receive care.
Tom Temin: And are these two major contractors responsible for the quality of the care that’s delivered?
Sharon Silas: Yes. Ultimately, VA is responsible for ensuring that veterans are receiving quality care, but because the contractors are doing the credentialing and the screening of the providers that will be participating in the network, the contractors play an important role.
Tom Temin: Alright. So you found a flaw in those contracts, and that’s the ability to track licensing.
Sharon Silas: Yeah. So we reviewed both of the contractors contracts and their policies that should outline the process that the contractor should be using to ensure that those mission ask restrictions are properly implemented, and to ensure that the providers that are participating in the community care network are qualified and providing safe health care. But what we found was that only one of the two contractors had a process in place that included verifying the providers licensure histories, and neither the contractors had a process in place to do continuous monitoring of the providers licenses.
Tom Temin: Well, these large contractors Optum and TriWest, what else do they do in life? That is to say, do they provide this kind of intermediary service for other organizations? Or were they set up simply to serve VA, and therefore might not have had this basic mechanism to check the licensure history of the providers?
Sharon Silas: No, the contractors actually already had some of the network in place. So for example, TriWest was already participating as a contractor with VA. Optum is a new contractor that VA is working with for the Veterans Community Care Program, but they also are contracted out to provide a network of services to other providers.
Tom Temin: But Optum and TriWest, they have other clients besides VA?
Sharon Silas: Yes, that’s correct.
Tom Temin: Are there other clients federal, like the military?
Sharon Silas: It could be, or it could be other health care networks that they’re providing a network of providers for.
Tom Temin: So therefore we know they can’t track the licensure history, so I imagine that’s your do now recommendation.
Sharon Silas: That’s correct. We made three recommendations in our review. The first was for VA to require the contractors to amend credentialing policies to ensure that the providers who have lost a license are unable to participate in the community networks. And the second recommendation was for VA to require the contractors to develop and implement a process that allows for continuous monitoring of the Mission Act requirements, even including considering some employing tools that can help facilitate the ongoing monitoring. And then we also made a recommendation that VA should identify, analyze and respond to the rest of unqualified providers participating in the Veterans Community Care Program.
Tom Temin: Are there any reports of unqualified practitioners participating? Like somebody that’s a palm reader that’s acting as a chiropractor or something.
Sharon Silas: So the Veterans Community Care Program was implemented as of June 2019. And one of the requirements in the Mission Act was that VA was supposed to begin tracking and eligible providers once the program was fully implemented. VA chose to track in eligible providers starting in May 2019, so that was one month prior to the implementation of the program. And while this met the requirements of the Mission Act, it really does continue to be a risk that providers removed from VA employment for quality care issues could still be providing care through the Veterans Community Care Program. So what we did in our review and our analysis, we went further back from May 2019, we went all the way back to 2016, and we identified providers that were potentially providing care through the Veterans Community Care Program. I should add that when VA looks back that one month, from May 2019 to identify ineligible providers, they did identify at least 136 providers which they removed from the system that they use to schedule appointments for veterans through the Community Care Program.
Tom Temin: Wow. So those people are out there, then they’re probably providing care to other people besides veterans under the VA. And just out of curiosity, are you aware of any linkage where the VA can call say a state authority or a local hospital chain and say, hey these people, we kicked them off, you might want to look at them, or that’s outside the scope?
Sharon Silas: So VA s contractors through the credentialing process can check various databases, such as state medical licensing databases or the national practitioner data bank, and check to see if there’s been a loss of license or if there’s any adverse actions taken against the providers. In our recommendations, particularly the recommendation that VA should use continuous monitoring, we suggest that potentially the contractors could use the national practitioner data bank, for example, to identify any providers that may have had any adverse actions or lost licenses.
Tom Temin: But I’m wondering if VA could use its own data and publish that if it got rid of 136 providers, I wonder if other health care networks would be interested to know what VA has done.
Sharon Silas: Sure. And as VA should be, if a provider has been let go from VA due to quality care concerns, VA should be reporting those providers to the national practitioner data bank where other health care networks or health care systems will be able to check to see if a provider is not qualified.
Tom Temin: And is it possible for veterans, is there a mechanism for them to report what they feel might be substandard care that would at least trigger VA to take a look at a provider?
Sharon Silas: Sure. There’s a process that veterans can go through. They can report a complaint they can, if there’s for example, a procedure that has gone wrong and the veteran has concern for that, there’s a whole process within the VA medical system that they can use to raise those concerns and have them investigated.
Tom Temin: Sharon Silas is director of Health Care Issues at the Government Accountability Office. Thanks so much.
Sharon Silas: Thank you.
Copyright © 2024 Federal News Network. All rights reserved. This website is not intended for users located within the European Economic Area.
Tom Temin is host of the Federal Drive and has been providing insight on federal technology and management issues for more than 30 years.
Follow @tteminWFED