Solving VA’s problems, one innovative idea at a time
The VA's Innovation Demo Day highlights ideas and inventions to help serve patients and support employees.
More than 4,000 miles separate Alaska and Louisiana, but the two states are working hand in hand to engage and retain Veterans Affairs Department employees.
Amy Thames of the Alexandria VA Health Care System in Louisiana, and Roxanne Nilsson of the Alaska VA Health System, are leading JumpStart onboarding efforts in their respective medical centers, and they came to Washington, D.C. to talk about their progress during the VA Innovation Demo Day.
“Basically, what this program is, is an onboarding program that has a two-pronged or three-pronged effect depending on the facility that you’re working with,” said Thames, a health systems specialist and executive assistant to the associate director for patient care services. “For Alexandria, it was the creation of a webpage for our new employees. So when they get their tentative offer, they actually can go onto this webpage and see what’s required, what to do the first day, where to park, different things. And then after, when they actually come on board and start new employee orientation, they will actually have a mentor assigned to them for the first eight weeks. This mentor will do kind of whatever they need: tours of the facility, questions they may have, concerns, anything they might have that they may not necessarily be comfortable talking [about] with other coworkers or their supervisors.”
For Anchorage, JumpStart was more for recruitment and retention, said Nilsson, currently the education technician for the Alaska VA and soon to be administrative officer for facilities management.
“We are an outpatient facility-only in Alaska, so we have a few different challenges,” Nilsson said. “One of our major ones is a sense of isolation being in Alaska. So the JumpStart mentor helps a lot in just them feeling more comfortable and more like they’re part of our team coming into a brand new state and facility.”
While the uses — not to mention the physical distance — range widely, JumpStart is a program helping to improve both the workforce environment at VA, and in turn the services it provides to veterans.
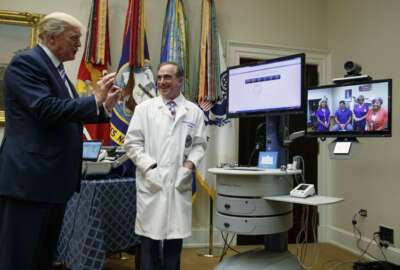
That’s at the heart of VA’s Innovation Demo Day, said VA Secretary Dr. David Shulkin, who spoke at the Aug. 8 event.
“This forum is essential to finding new ways to improve the lives of those who have served, and why it’s critical to tap into the remarkable wealth of creative and technological ideas of our VA employees,” Shulkin said.
The department piloted the VA Innovators Network with eight medical centers across the country in 2015.
The Innovators Network has three funding routes. They are:
- spark grants, which assist innovation teams to do more testing on their ideas and help them narrow down individual projects.
- seed grants, which give innovators a chance to test and finalize their ideas.
- spread grants, which help innovators share their ideas and make them VA medical centers’ best practices.
Shulkin spoke to the standing room only crowd gathered at Georgetown University about the VA’s top five priorities: greater choice, modernizing VA systems, improving timelines, investing in foundational services and eliminating veteran suicide.
VA is also looking at 13 areas where the department needs to improve and the legislative and administrative fixes it needs in order to see progress.
“This is really where we need you to innovate on,” Shulkin said. “This is going to be the way that we solve VA’s problems and make us a sustainable, stronger system for our country’s veterans; one that I believe is absolutely essential to our national security for us to fulfill this mission.”
Reducing veteran suicide
Katherine Luci and Lauren Hagemann, both of Virginia’s Salem VA Medical Center, are working to address veteran suicide through their awareness project aimed at veterans leaving Community Living Centers (CLCs).
Luci, a clinical juro-psychologist at the Salem facility, said it was encouraging to hear Shulkin directly address veteran suicide, because the veterans she works with — those 60 and older — don’t get as much attention. However, veterans over 65 who’ve gone through a health crisis are 36 times more likely to commit suicide, she said.
Latest Veterans Affairs News
Several years ago VA published a memo about the increased risk for suicide in veterans who are discharged from a CLC, which can be a combination of long-term care like a nursing home and a place for short-term rehabilitation.
“A lot of times the CLC psychologist never sees the veteran before they get discharged,” Luci said. “And there’s high turnover and they’re very busy and it’s very difficult to provide appropriate follow up.”
After the memo was published, the nationwide community of CLC mental health providers began talking online about how to address this risk.
Today the Salem medical center is piloting a program in which the primary mental health care provider calls the veteran one week after their discharge, and calls again to check up on the veteran at the 30-day mark.
“Just to see how the patient is adjusting,” Hagemann. “Are they requiring any more supports or services, and we kind of bridge that gap. We’ve had a few patients who requested referrals to mental health clinics or caregiver support. We’ve been able to bridge the gap for them. After the 30-day call, I do a little bit of a program evaluation, asking the patient or the caregiver … just getting their feedback; if the call was helpful for them, if they have any recommendations.”
Hagemann said the response has been overwhelmingly positive, and one of the most common requests is for a 60-day call.
PTSD remission
Another person encouraged by Shulkin’s comments was Sheila Rauch, director of research and program evaluation at the Atlanta VA Medical Center.
Rauch’s work addresses Post-Traumatic Stress Disorder, and Brief Prolonged Exposure [remembering/re-experiencing a traumatic event] as a therapy choice for veterans. Rauch said she’s been working on this concept for a decade.
“We know that most patients with PTSD never actually get to specialty mental health, to get the treatments that work best for that disorder,” Rauch said. “So we wanted to bring those treatments in effective form right into primary care, which is where most of them actually present for care.”
Rauch said through the program, primary care doctors or nurses can immediately contact embedded mental health providers who work within primary care, and that same day can get their patient started in four 30-minute sessions.
Rauch said she’s seen a 41 percent remission rate in the patients who go through the intervention, and something like the VA Innovation Demo Day helps highlight the work being done — and in turn gather support and resources to help with training and making a more efficient program model.
“I hear everything that Secretary Shulkin’s saying,” Rauch said. “I think this intervention actually fits really well with a lot of the priorities that he mentioned. Definitely with access, reducing suicide, any time we can treat mental health disorders potentially to remission, is going to help us with all of those outcomes.”
Copyright © 2024 Federal News Network. All rights reserved. This website is not intended for users located within the European Economic Area.
Related Stories





